Nursing and Residential Care Homes
multi-disciplinary teams
Keywords: Primary care, care homes, medical services, quality of care, interprofessional cooperation
Family Doctors contracted as staff members in care homes
Summary
What is the main benefit for people in need of care and/or carers?
What is the main message for practice and/or policy in relation to this sub-theme?
Warum wurde diese Initiative implementiert?
Primary (and specialist) medical care in care homes in Germany is often criticised as underdeveloped. Residents and staff suffer from an undersupply of medical care, since family doctors (specialists even more so) delay or refuse home visits for immobile residents, mostly because of low remuneration through disincentives and structural governance problems. Having a loosely connected and changing group of family doctors (‘every resident chooses his/her doctor’) hinders stable communication routines between medical carers and nursing staff. Establishing standards is difficult since there is no defined medical responsibility for the institution.
The project responds to these problems by introducing an organisational change: family doctors are employed or contracted by individual care homes to supply residents with continuous medical care. Therefore, in contrast to ‘on demand’ cooperation with local doctors, ‘care home doctors’ are part of the care home staff. Routine weekly visits and team conferences grant both care staff and residents enhanced accessibility to medical care. Since the employed doctors are accountable for whole care home populations, cooperation with staff is promoted: they identify more with the care home organisation. For example they feel more responsible for the development, implementation and quality control of medical standards and guidelines within the team, whereas care homes working with different doctors often complain about varying and sometimes contradictory instructions concerning intervention standards.
Beschreibung
In 1998 several regional health insurance organisations, BKG, VPKBB and the local association of statutory health insurance physicians in Berlin concluded a framework agreement addressing the introduction of accountable “care home doctors” in several care homes in Berlin. The initiative was a response to a historical change, as the types of care homes that had existed since the 1970s in former West Berlin and which had worked with employed doctors had to be transformed to conform to the new legislation (and financing arrangements) of the care insurance system introduced in 1994. Several care homes in the region voluntarily took part in the project. Since 1998, 38 care homes have been involved, 27 of them employed family doctors as staff members (24/7 services, on call), 11 others contracted family doctors in the community to provide services in the home (weekly visits, services for about 30-40 residents, on-call shifts, multiprofessional team meetings, standardised documentation). Residents retained the right to choose their own doctor. These new standards led to better access and quality improvements in primary care delivery in the participating care homes.
One important characteristic of the project was its innovative financing concept: Every care home provider received a fixed budget from the respective health insurance to ensure medical care for the insured residents. Bonuses were paid if the budget was not utilised. Despite not all health insurances participating, the employed care home doctors were often responsible for all residents, irrespective of their kind of insurance. The care home providers involved were motivated by perceived quality improvements which also appeared to act as competitive advantages in the LTC market. Employed or contracted family doctors were motivated by higher remuneration (capitation, bonus-malus-system) than in individual practice.
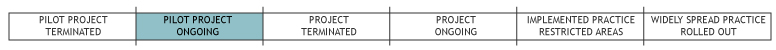
Because of its success and public recognition the project has been extended several times. Decisions about the future of the “Berliner Projekt” are currently in negotiation. According to the main initiating health insurer (AOK Berlin) negotiation will soon come to an end. In 2007 AOK Berlin established a parallel-running follow-up project (“careplus”, involving currently 31 institutions), to enable additional care homes for an improved primary care service for their residents. Careplus is based on a new contracting option for integrated care introduced by the latest German health care reforms (§140a SGB V, GKV-Wettbewerbsstärkungsgesetz 2007). In this project, free choice of doctor is restricted and only residents who are members of the initiating insurance scheme receive services. Physicians receive extra fees besides their budgets if they are partners in the project.
Welche Effekte wurden erzielt?
An independent external agency has conducted regular evaluations of the care homes participating in the ‘Berliner Projekt’ using data on a) actual costs (from health insurers) and b) residents’ health status (according to the standardised Resident Assessment Instrument, RAI). Cost-control reports were supplied to care homes quarterly, quality reports based on RAI annually. Participating care homes appear to provide primary medical care more continuously and efficiently (see references below, plus: partly unpublished data, personal communication by AOK Berlin):
- Better medical care: Deteriorating health of residents was detected earlier and emergency scenarios could often be avoided. Hospital admissions decreased significantly in the participating care homes. Prescriptions of medication were lower (a typical effect of a holistic geriatric approach). Cooperation between medical and care staff was better and more direct.
- Greater satisfaction: Residents, relatives and staff reported greater satisfaction with services, which were seen as more accessible and more reliable.
- Economic savings: Despite significantly higher costs for medical staff the project still produced economic savings. The main savings were attributable to reductions in patient transports, medication and hospital admissions. For 2009 the health insurers report savings of about €1.5 million, or about €617 per resident.
Worin bestehen die Stärken und Schwächen der Initiative?
Strengths
- The project represents one of the most successful approaches in Germany for improving medical care for care home residents, who are a hard-to-reach group in the German care system: despite their being institutionalised, these patients receive insufficient medical care if their individual mobility is limited and visits to a physician’s practice are difficult.
Weaknesses
- The limitations of the project largely concern the provision of specialist medical services, which are still reported as undersupplied in care homes.
- The project cannot overcome structural barriers such as financial disincentives (underpayment of home visits).
- Qualification problems for the contracted physicians also seem to have presented a challenge, as geriatric qualification of physicians is still a developing field in Germany.
Opportunities
- The concept of a contracted/employed care home doctor is widely recognised in current LTC policy debates in Germany. As a result it has been included as an option for care homes in the latest legislation, the Long Term Care Further Development Act (2008). After pilot-testing in Berlin, it remains to be seen whether these new options will lead to similar initiatives in other German regions.
Threats
- It was not easy to acquire physicians as care home doctors (shortage of qualified doctors, lack of financial incentives, problems of professional culture where geriatric care is rather low-status).
- Care home providers hesitate to take financial responsibility for medical services, since this is a new reform-driven option where they lack experience.
- The physicians’ association is not interested in expanding a project with fixed budgets (lack of financial incentives).
- An important barrier to general implementation is created by the recent health care reform, which introduced competition between health insurers. Insurers use the project to sharpen differentiation and secure competitive advantages. It is therefore rejected by health insurers who do not participate. The resulting mixture of participating and non-participating residents within care homes (depending on their insurer) exacerbates the organisational complexity and challenges for the home providers (different budgets, regulations) and thereby reduces their motivation to take part.
Impressum
Autor: Anja DieterichReviewer 1: Marion Repetti
Reviewer 2: Kerry Allen
Verified by: Sabine Hochstadt, AOK Nordost - Die Gesundheitskasse
Links zu anderen INTERLINKS-Initiativen
- Cité-Générations - A care network including sheltered housing
- Greek Care Homes Association (PEMFI)
- www.Heimverzeichnis.de: Certified quality of life in nursing homes
Externe Links und Literatur
- Berliner Projekt
- Project 'Careplus'
- Hallauer, J., Bienstein, C., Lehr, U. & H. Rönsch (2005) SÄVIP - Studie zur ärztlichen Versorgung in Pflegeheimen. Hannover: Vincentz Network Marketing Service.
- Kotek, H. (2005) 'Acht Jahre „Berliner Projekt“ in der stationären Pflege: Hohe Qualität, weniger Kosten', pp. 51-58 in: Füsgen, I. & J.F. Hallauer (eds.) Zukunftsforum Demenz: Demenzbehandlung in Pflegeheimen – Wirklichkeit, Chancen und Grenzen. Geisenheim: Zukunftsforum Demenz.

