Care from a Hospital Setting
multi-professional teams for assessment, care and treatment
Keywords: geriatric medicine, assessment, remobilisation, multi-professional care, acute care
Geriatric Acute Care and Remobilisation Units
Summary
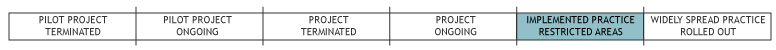
Approximately 40 Geriatric Acute Care and Remobilisation Units (AG/R) have been integrated within public hospitals in six out of nine Austrian provinces since the year 2000. AG/R units are currently established as independent clinical departments under the lead of specialists in Internal Medicine or Neurology, with some of the units also running a related day clinic. A continuously growing share of older patients with multifaceted health problems and a still lacking academic specialisation in geriatric medicine in Austria were the main drivers for the development of AG/R. The further development of AG/R in Austria is supported by relatively strong political commitments and a related national plan concerning the implementation and expansion of AG/R facilities in Austria (GÖGmbH, 2010). Since 2008 a benchmarking process based on existing data of treatment and rehabilitation processes and indicators for structural quality in AG/R units is underway. First evaluation reports are expected by 2011.
What is the main benefit for people in need of care and/or carers?
Based on a comprehensive assessment process, AG/R units offer specialised but multi-professional treatment and remobilisation combined with timely planning of discharge, reintegration and follow up procedures. Respecting individual needs, social context and existing (in-) formal networks of older people in need of acute clinical treatment are basic objectives of AG/R.
What is the main message for practice and/or policy in relation to this sub-theme?
Multiprofessional services, which allow to combine specialised geriatric medicine, care and remobilisation as well as measures of social reintegration are of need, as we are facing a growing number of older people with complex health and care needs.
The growing demand for and positive experiences with AG/R facilities contribute to an on-going discussion in Austria about the still missing implementation of an academic specialisation (combined with the respective curriculum) in geriatric medicine.
Why was this example implemented?
Specific needs of geriatric patients are not yet sufficiently met within the currently provided acute health care structures in Austria. Therefore, in 1999 an expert panel, assigned by the Austrian Federal Institute for Health Care (ÖBIG), proposed the plan for a network of Geriatric Acute Care and Remobilisation units –Akutgeriatrie/Remobilisation (AG/R) – all over Austria.
The basic objective of AG/R units is to provide specialised and at the same time multi-dimensional and community related services to older patients based in a clinical context. In general, services are directed towards older people who are suffering from somatic and/or psychic multi-morbidity, who are limited in their autonomy due to functional or cognitive disorders or psychosocial problems and last but not least towards those who are in need of rehabilitative and re-integrative measures (ÖGGG, 2008). Central principles of AG/R units are individually adapted treatment and rehabilitation plans, early remobilisation and planning for social reintegration as well as co-ordination with services and support networks in the community.
AG/R units can thus address gaps and interfaces between different professional groups within the hospital setting (e.g.: medicine, nursing, occupational and physiotherapy, dieticians, logopedics etc.) and – via discharge management – between clinical, rehabilitation and follow-up services such as day-clinics, professional home-care organisations etc.
Description
The plan for a network of Geriatric Acute Care and Remobilisation units in Austria was adopted in 2000 by the Austrian Federal Institute for Health Care. The Austrian Structural Plan for Health defines the framework conditions, necessary capacities and the official quality standards for Geriatric Acute Care and Remobilisation units in hospitals. These criteria comprise minimum personnel requirement, adjustment of hospital infrastructure to the needs of older people (technology and room equipment, size), and the services required. The most recent revision of this plan was performed in the year 2010 (GÖGmbH, 2010). The systematic implementation and gradual expansion of AG/R facilities in all regions of Austria was assigned to the regional health planning authorities.
As there is no professional specialisation in Geriatric Medicine in Austria so far, Geriatric Acute Care facilities are usually established under the lead of a specialist in Internal Medicine or Neurology, who need to hold an additional diploma in geriatrics (courses are currently launched by the Austrian Medical Chamber).
A multidimensional treatment regime is offered to patients in primary (admission from the community) and secondary (transition from the same or another hospital) Geriatric Acute Care and Remobilisation units. A core element and tool of all AG/R facilities is a standardised and comprehensive geriatric assessment, which aims to estimate the general physical potential and functional abilities of a patient and to use this information in a following process of comprehensive treatment, care and remobilisation. The duration of treatment and care in AG/R units is limited to a few weeks with the basic intention to discharge the patients afterwards to his/her private surrounding or to allow for further and specialised rehabilitation. By offering professional discharge management AG/R can provide basic support to patients and their families at the moment of discharge when professional home care and follow-up treatment becomes necessary.
Some AG/R units in Austria can also offer ambulatory (follow-up) treatments and specific therapies in attached day clinics.
Accounting for costs of clinical services within AG/R is generally regulated by the DRG-system. As AG/R are integrated in the public hospital structures of Austria and their complex system of financing, a separate specification of costs for AG/R services was not available for this description.
What are/were the effects?
So far approximately 40 units for Geriatric Acute Care and Remobilisation (i.e. approx. 1,440 beds) have been established in six of nine Austrian provinces (GÖGmbH, 2010).
In general, the on-going implementation of AG/R units in Austrian hospitals does not only allow for a specialised and at the same time comprehensive clinical assistance to older people, but also improves the general awareness for the specific and multi-layered medical, psychological and social needs in geriatric health care. Such kind of specialisation and awareness consequently leads to more multi-professional cooperation and professional links within the hospital unit (multi-professional geriatric teams) and via better discharge management also with external and follow-up services (provided at home, in a related day-clinic, a rehabilitation centre, a nursing home etc.).
The availability of specialised but at the same time comprehensive clinical services for older patients with multiple health problems is obviously to the advantage of users and carers alike. However, only one (rough but generally positive) evaluation dealing with four AG/R facilities in the city of Vienna was published by the Austrian Audit Court in 2006 (Audit Court, 2006).
The comprehensive geriatric assessment has been standardised and since 2008, data of treatment and rehabilitation processes as well as indicators for structural quality of the clinical facilities have been used for a first benchmarking of Geriatric Acute Care. Initiated by the Austrian Society for Geriatrics and Gerontology, currently AG/R units in four Austrian provinces (K, OÖ, St, W) are fully and voluntarily participating in the related benchmarking process guided and evaluated by “Joanneum Research Austria” together with the society QIGG. First evaluation reports based on the benchmarking process should be public by 2011.
In some European countries specialised geriatric care in hospitals already exists in a comparable and advanced form. However, there are usually remarkable regional differences concerning quality standards and degree of implementation. Generally, there are no apparent problems in transferring the basic idea of AG/R unit as well as related structural and quality requirements from one country to another. As always the practical implementation of the theoretical framework will depend on the organisation of the national/local health-care system and respective regulations in governance and financing.
What are the strengths and limitations?
AG/R units can facilitate transition processes and take the wider social circumstances of a patient into account. However, there are still remarkable difficulties and gaps concerning collaboration and communication with informal carers and external service providers. All in all AG/R units represent important achievements, starting points and models for the future provision of comprehensive geriatric care in Austria.
Strengths
- existing political commitment
- national plan of implementation and graded expansion
- comprehensive and multidisciplinary approach within the clinical context
- awareness of the social context and of individual patients’ pathways
- focus on activating care, early remobilisation and social reintegration
Weaknesses
- insufficient or selective cooperation (e.g. only within the network of the same public providers) with external providers of medical and social care (GP, homecare services, 24-hour carers, mobile physiotherapy, informal/family care etc.)
- imbalances between medical and rehabilitative services (depending on AG/R unit)
- no combination with mobile geriatric teams
- insufficient national expansion
- lack of comprehensive evaluation
Opportunities
- further national expansion
- combination with mobile geriatric teams/(nursing)home visits
Threats
- on-going lack of special education and sufficiently trained medical and nursing staff
- possible negative influence on individual care planning by standardised hospital routine and related organisational ideologies
Credits
Author: Georg RuppeReviewer 1: Laure Com-Ruelle
Reviewer 2:
Verified by:
External Links and References
References:
- Austrian Audit Court (2006)
- GÖGmbH (2010), Österreichischer Strukturplan Gesundheit 2010. ÖSG 2010. Wien: BMG.
- ÖGGG (2006), Basisassessment. An einem Strang ziehen. In Geriatrie Praxis Vol. I.
- ÖGGG (2008), Positionierung älterer Patienten im Gesundheitswesen. Strukturelle Voraussetzungen für die stationäre Geriatrie. Medizin Medien Austria: Wien.
Selected Links:
- http://www.oegkv.at/fileadmin/docs/OEPZ_2002/10/fellinger.pdf
- http://www.goeg.at/de/Bereich/Akutgeriatrie-Remobilisation-Begleitung-und-Steuerung.html
- http://www.medizin-medien.at/dynasite.cfm?dsmid=72613&dspaid=561354
- www.qigg.at
More information on the “Austrian Basic Geriatric Assessment”:
The so called “Austrian Basic Geriatric Assessment”, as adapted and recommended by the “Austrian Society for Geriatrics and Gerontology” aims at a comprehensive evaluation of a patient’s health and general condition. The multidimensional examination, ideally performed by a multidisciplinary team comprises and evaluates five dimensions namely physical, psychological, social and economic as well as self-help abilities of the older patient. In clinical examinations a minimum of six different parameters are usually used and tested: (1) ADL, (2) IADL, (3) mood, (4) cognition, (5) nutrition, and (6) mobility. For each parameter two different instruments of testing are up for election when performing the standardised assessment (ÖGGG, 2006).

