Specialised Case or Care Management Centres
structures that facilitate multi-professional and inter-agency care planning and coordination
Keywords: Dementia, case manager, informal care, integrated care
Case managers for people with dementia and their informal caregivers
Summary
Many people with dementia and their caregivers do not really know how to deal with dementia and where to find the right help. Informal caregivers need additional information and advice, e.g. about how to cope with their relatives’ behavioural problems and about the development of the illness trajectory.
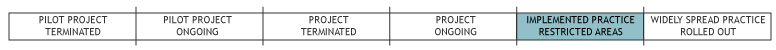
From 2004 until 2008 an experiment was initiated by the National Dementia Programme (LDP) with sixteen frontrunner regions from the Netherlands, where co-operation in community dementia care would be put into practice and case managers were introduced to coordinate the care for dementia clients. It was left to regions to bring about the required cooperation within the region, for example with home care organisations, general practitioners, geriatricians, psychologists, etc. from a multidisciplinary team. By the middle of 2010, the experiment had been rolled out to 57 regions, based on experiences from the frontrunner regions. The implementation of case managers was the most important consequence of this experiment.
The case manager sets up a diagnosis trajectory, coordinates the care provided and informs and advises the client and caregiver. In this way, the case manager meets their specific needs.
What is the main benefit for people in need of care and/or carers?
The main benefit of case management is its positive effect on the client’s wellbeing, the informal caregiver’s burden and delayed admission to a nursing home.
What is the main message for practice and/or policy in relation to this sub-theme?
For implementation of case management in dementia care it is advised to standardize financing, training and practice (i.e. number of clients per case manager, case management combined in a multidisciplinary geriatric team cooperating parties).
Why was this example implemented?
Case management has been an effective treatment in psychiatry for a long time: it has a positive effect on clients with chronic problems and prevents admission to institutions. In the past decade, some regions started to provide case management for people with dementia and their caregivers. However, there was no golden standard. Moreover, the funding of case managers was almost always temporary. Therefore, the Ministry of Health, Welfare and Sports initiated an experiment, the National Dementia Programme (LDP). The goal was to realise structural funding of case management as part of a collaboration with all parties involved in dementia care in a region on the basis of special (integrated) funding by regional offices of the public LTC-insurance. Sixteen frontrunner regions acted as models for others, although every region was responsible for the outline of their own policy regarding funding, care provided and cooperation within the region. Despite this variation in implementation, case managers always provide client-orientated care, which is especially important for dementia clients and their informal caregivers, who often do not know where to find the right help. They have a central position in the collaboration with multiple health (and sometimes social) care providers and integrate them into a chain, to realise continuity and coordination of care.
Description
Geriant is an independent care organisation for dementia diagnosis, treatment and care, that started providing case management for dementia as one of the first organisations in the Netherlands. Many regions used Geriant as an example. Nowadays, dozens or other organisations throughout the Netherlands provide case management. The manager of an organisation for mental health care wanted to improve dementia care and used the concept of case management from the field of chronic psychiatry. Multidisciplinary teams, called DOC-Teams (dementia examination and case management teams), were formed consisting of case managers (about 10), geriatricians (2), a psychologist and a dementia consultant, funded via diagnosis treatment combinations (DBC’s). This is a standard amount of money that an insurer provides and that is linked to a certain diagnosis (and treatment). Four DOC-Teams are now operational in different geographical area’s in The Netherlands. They cover 25 towns and a population of 600,000 people. A general practitioner, or anyone else with the general practitioner’s agreement) can refer people with suspected dementia to a DOC-Team. This can also be an informal caregiver or the client.
The DOC-Team starts a diagnosis trajectory, usually at a location of Geriant, but diagnosis at home is possible. New clients are discussed within the DOC-Team every week. Within two weeks, the results of this meeting: a diagnosis and a care and treatment plan, are presented to the client and informal caregiver. The case manager is the executor of this plan, informs and advices the client and informal caregiver and coordinates the consultation of other professionals. This is especially important for dementia clients, who often don’t realise they need help and don’t know where to find it.
All casemanagers are originally nurses or social workers and have experience with psycho geriatric clients. They have a caseload up to 70 clients (1 fte, fulltime-equivalent), which is seen as heavy. Nationally a caseload of 50 clients is considered as a maximum. Several training courses for case managers are being developed and implemented. The contact between the DOC-Teams and other health care professionals and organisations is very good, because both health care professionals and managers realise they need each other in reaching their common goal: the best care for the dementia clients and best support for the informal caregiver. This has resulted in a coordinator (one of the case managers) who can, in case of a crisis situation, place people in a nursing home immediately. People who need to be hospitalized, but have specific psychogeriatric problems, can also be transferred to the Geriant DOC-centre for crisis situations. For more information (in Dutch only) click here.
Besides Geriant, there are dozens of similar examples providing case management in The Netherlands. They mainly differ in the way case management is funded (e.g. insurers, Exceptional Medical Expenses Aid (AWBZ), subsidy, diagnosis treatment combination), which cooperating parties are involved and how, and whether clients are referred to the case manager before or after diagnosis. However, as a main responsibility all case managers inform and advise the client and the informal caregiver, as well as coordinate the care provided.
What are/were the effects?
Evaluation research has shown that clients and particularly informal caregivers are satisfied with the help from their case managers (Groenewoud, 2008; Ravensbergen, 2006; Stichting Geriant, 2008; Werkman, 2010). Their interventions have a positive effect on the clients’ mental health (Callahan, 2006; Counsell, 2007), general health and vitality (Counsell, 2007) and decrease the burden of the informal caregiver (Challis, 2002; Chien, 2008; Cox, 2001). Furthermore, case managers are the catalysts of integrated dementia care with collaboration between different health care professionals such as general practitioners, psychologists, nurse practitioners, etc. (Ligthart, 2006). The executors of the LDP assume that case managers can have a positive effect on health care costs by preventing respite care and postponing admissions to residential or nursing homes. Because informal caregivers are supported and less burdened, they are able to take care for the dementia client at home for a longer time. More and more health care managers, politicians and insurance offices recognize the positive effects of case management. This will lead to structural ways of funding, also because from the year 2011, every dementia client will have the right to be supported by a case manager.
It is not clear at this moment from what source case management will be funded. When the LDP first started in 2004, sixteen frontrunner regions implemented case management. After 4 years, 57 regions had done so, covering 90% of the Netherlands. Still, new initiatives are being developed and existing initiatives improved.
What are the strengths and limitations?
Strengths
- Concept of case management
- Client-oriented care
- Caregiver and client satisfaction about case managers is high
- Case managers reduce the burden on caregivers
- Admissions to nursing homes are postponed
- Decrease in use of respite care
Weaknesses
- In the Netherlands: the way case managers are funded
Opportunities
- Case managers combined in a multidisciplinary geriatric team are more effective
- Study on case management for people with dementia shows that the motives, aims and main characteristics of case management are comparable
- More and more policy makers and managers are seeing the importance of case management
Threats
- The surplus of case management is clear to most people, but not to everyone. Especially general practitioners and municipalities are not always involved in the collaboration
- Case managers face a very high case load
Credits
Author: Sabina MakReviewer 1: Francesca Ceruzzi
Reviewer 2: Kai Leichsenring
Verified by:
External Links and References
- Callahan CM, Boustani MA, Unverzagt FW, Austrom MG, Damush TM, et al. (2006) 'Effectiveness of Collaborative Care for Older Adults with Alzheimer Disease in Primary Care: A Randomized Controlled Trial' in: JAMA; Vol 295(18):2148-57.
- Challis D, von Abendorff R, Brown P, Chesterman J, Hughes J (2002) 'Care Management, Dementia Care and Specialist Mental Health Services: An Evaluation' in: Int J Geriatr Psychiatry, Vol 17:315-25.
- Chien WT, Lee YM (2008) 'Disease Management Program for Families of Persons in Hong Kong with Dementia' in: Psychiatr Serv, Vol 59(4):433-6.
- Counsell SR, Callahan CM, Clark DO, Tu W, Buttar AB, et al. (2007) 'Geriatric Care Management for Low Income Seniors: A Randomized Controlled Trial' in: JAMA; Vol 298(22):2623-33.
- Cox C, Albisu K (2001) 'The Alzheimer's Connections Demonstration Program: Instituting A National Case Management Program' in: Am J Alzheimers Dis Other Demen, Vol 16(5):279-84.
- Groenewoud H, Egers I, Pool A, Lange J de (2008) Evaluatieonderzoek van de pilot casemanagement dementie in regio Delft Westland Oostland 2005-2007, eindrapport. Rotterdam.
- Ligthart S (2006) Casemangement bij Dementie. CBO.
- Ravensbergen C, van Slooten E, van Wensum I (2006) Eindrapportage casemanagement dementie. Leiden: RCG ZHN.
- Stichting Geriant (2008) Cliënttevredenheidsonderzoek 2008.
- Werkman W, Lensink E (2010) Ketenzorg dementia vanuit cliëntperspectief - Bevindingen eerste meting Cliëntenmonitor Ketenzorg Dementie, Onderdeel van de Cliëntenmonitor Langdurige Zorg. NPCF & Alzheimer Nederland.
Websites:
- www.geriant.nl (Dutch only)

