Formal Care in the Home and Community
multi-professional teams (eg preventive/rehabilitative measures)
Keywords: Domiciliary rehabilitation, multi-morbidity, interdisciplinarity, social par-ticipation, quality of life
Domiciliary Rehabilitation (MoRe)
Summary
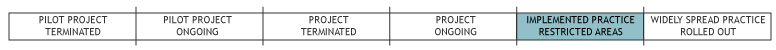
Domiciliary Rehabilitation (DR) is an innovative form of outpatient rehabilitation, which since 2007 has been acknowledged as a service that is refundable by the Social Health Insurance. However, so far it is only running in five places in Germany. Patients with multiple morbidity including severe functional limitations are the DR target group, mainly old and very old people. DR means rehabilitation of the patient in his or her own home, delivered by a multidisciplinary team led by a physician. It aims at improving patients’ activities of daily living (ADL) and instrumental activities of daily living (IADL). Located in the patients’ home and neighbourhood, the DR team can take into account the contextual factors affecting patients’ care situation and functioning, such as the home environment and informal care relationships, and maintain and enhance social inclusion. The quite slow increase and further spread of the provision of DR in Germany refers to low financial attractiveness and enduring traditions in geriatric rehabilitation.
What is the main benefit for people in need of care and/or carers?
What is the main message for practice and/or policy in relation to this sub-theme?
Why was this example implemented?
The background for the development of DR was the lack of rehabilitation programmes/services for the target group with complex needs such as those listed below (see description) who often do not get access to rehabilitation. The consequences of this service gap were that the rehabilitation potential of the target group was not addressed, and that admissions to care homes could be avoided with respective consequences regarding costs and quality of life.
Patients with multi-morbidity including severe functional limitations therefore are the target group of DR, mainly old and very old people. DR means rehabilitation of the patient in his or her own home, by specific multi-disciplinary physician-led teams. The main goals are rehabilitation of functioning (ADL – Activities of Daily Living: self-care activities such as personal hygiene and grooming, dressing and undressing, feeding oneself, functional transfers; and IADL – Instrumental Activities of Daily Living: housework, meal preparation, taking medications, managing money, shopping), social participation and quality of life as well as prevention or postponement of care home admissions. Located in the patients’ home and neighbourhood, the DR team can take into account the contextual factors affecting patients’ care situation and functioning, such as the home environment and informal care relationships, and maintain and enhance social inclusion.
DR is given to patients who for various reasons (mental health problems and the risk of deterioration, fear of hospitalisation, care and other family responsibilities of the patient) cannot attend established forms of rehabilitation, or are not included in their target groups.
Description
DR is mainly targeted to geriatric patients, however, also to younger people with severe, complex and specific health problems.
The first initiatives started in the 1990s, partly within federal pilot programmes for care innovation by the Ministry of Health (BMG) and the Ministry for Family, Seniors, Women and Youth (BMFSFJ). In October 2010, it was provided in 5 places: Marburg, Woltersdorf, Karlsruhe, Bad Kreuznach, and Chemnitz. Others are still in negotiation.
Criteria for inclusion into this programme are having the potential to gain from this type of rehabilitation; multi-morbidity including dysfunction in mental health (cognitive and/or behavioural), or in voice and speech, sight or hearing; being dependent on the support of an informal carer; being unable to gain from or to participate in other forms of rehabilitation (for medical, psychosocial or other reasons such as fear of hospitalisation, care and other family responsibilities of the patient).
Preconditions for receiving the programme include a comprehensive assessment including medical, social and other context criteria such as suitability of the home environment; social care provided; active involvement of patient and informal carer.
Costs: Since 2007 DR is acknowledged as a service that is refundable by Social Health Insurance; therefore the regular copayment for patients is €10 per day for 20 days.
The team consists of a medical doctor, occupational therapist, speech & physiotherapist, nutritionist, specialist nurse, neuropsychologist, and social worker, all managed by a medical doctor.
Comprehensive assessment, case management, joint care planning and inter- and trans-disciplinary working are essential parts of the DR programme as well as promoting activities, social participation and community orientation of patient and carer. DR normally takes between 6 and 14 weeks; in individual cases it can be longer.
What are/were the effects?
First of all, DR provides rehabilitation to patients who do not regularly have access to rehabilitation, but do have significant needs for rehabilitation and the potential to gain from it.
Secondly, there is some descriptive evidence of the effectiveness of several DR programmes regarding functional improvements (Barthel Index – BI, Functional Independence Measure – FIM, IADL) (Schmidt-Ohlemann & Schweizer, 2008).
However, results regarding the other aims (see above) have not been evaluated and are difficult to measure.
Furthermore, it is not easy to compare this type of rehabilitation with others provided in Germany, either regarding cost-effectiveness or health and quality-of-life outcomes or preventable health care costs, since the target groups differ. Patients targeted by DR show significantly higher functional impairment prior to the DR compared to patients taking up outpatient or inpatient rehabilitation. Authors recommend research strategies linked to quality of life and social participation concepts, and to triangulate qualitative and quantitative methods (Schmidt-Ohlemann & Schweizer, 2008).
Regarding the costs, DR costs – for a complete intervention with about 45 treatment units – have been calculated as 50% higher compared to outpatient and 10% higher compared to inpatient rehabilitation interventions. However, the more complex mental, functional and psychosocial burden of DR patients has to be taken into account. (Schmidt-Ohlemann, 2010). Cost-effectiveness measures should also consider the wider social impact on patients and carers, and the long-term impact on health care and long-term care spending.
In Germany the legal situation for further development is positive. However, difficulties result from reluctance of social health insurers and the need for conceptual re-orientation (focusing on rehabilitation potentials of older people with LTC needs) on the side of providers and professionals. Thus this concept is slow to expand, although several new initiatives are currently being negotiated with insurers (Schmidt-Ohlemann, 2010).
What are the strengths and limitations?
Strengths
The concept has to be recognised for establishing a multi-professional effective intervention for geriatric patients who would otherwise not get access to rehabilitation and therefore would not have the opportunity to regain functional capacity and social participation.
Weaknesses
So far, DR is not well known among patients given the low uptake of its provision. A point for further discussion is that there is no formulated strategy regarding how DR will successfully link with the social care that is probably already present in many of the households.
Opportunities
Criticism of the approach concerns the missing professional infrastructure for appropriate rehabilitation services and potentially shorter treatment times which may create a shortfall in how rehabilitation progresses. A counter argument given is the greater opportunity of patients and carers for training activities of their own outside of treatment schedules and less transfer problems compared to other forms of rehabilitation (Schmidt-Ohlemann & Schweizer, 2008).
Threats
Proponents of the approach are concerned about implementation barriers so far. Social health insurers are reluctant to contract with regional providers in spite of the legal regulation. Moreover, where the service exists, individual assessment outcomes are often rejected and respective allowances denied. In fact, these are conflicts about costs – which contribute to the situation that many potential users do not have access to a flexible rehabilitation programme, meeting the needs of their complex life situations.
Credits
Author: Susanne Kümpers, Social Science Research Center BerlinReviewer 1: Georgios Kagialaris
Reviewer 2: Laure Com-Ruelle
Verified by: Carola Schweizer, Bundesarbeitsgemeinschaft MoRe (National Association for Domiciliary Rehabilitation), Saarbrücken
Links to other INTERLINKS practice examples
External Links and References
- Social Code (SGB V) Statutory health insurance
- Mobile Rehabilitation
- MoRe
- http://www.dvfr.de/fileadmin/download/Veranstaltungen/091106_MoRe/WS_MoRe_Schmidt-Ohlemann_aktueller_Stand_und_Wirtschaftlichkeit.pdf
- Schmidt-Ohlemann M, Schweizer C (2008). Mobile Rehabilitation: Eine Innovation in der ambulanten medizinischen Rehabilitation. Rehabilitation, 47, 1-11.
- Schmidt-Ohlemann, M. (2010). Mobile Rehabilitation: Eine Versorgungsform der Zukunft, Fortbildungsveranstaltung MdK Nord. Hannover.
- Schulz M, Behrens J, Schmidt-Ohlemann M. Ergebnisorientierte Evaluation eines Mobilen Rehabilitationsdienstes: Eine prospektive Studie. Phys Rehab Kur Med 2008 ; 18 : 30 – 34
- Meinck M, Robra BP. Abschlussbericht der Wissenschaftlichen Begleitung des Modellvorhabens: Aufbau ambulanter Versorgungsstrukturen in der geriatrischen Rehabilitation in Sachsen-Anhalt (AMBRA) . Magdeburg: Institut für Sozialmedizin und Gesundheitsökonomie, Otto-von-Guericke Universität Magdeburg ; 2003
- Schweizer C . Mobile Rehabilitation: Vom Modell in die Regelversorgung. Schriftenreihe zum Modellprogramm des Bundesministeriums für Gesundheit und Soziale Sicherung „ Verbesserung der Versorgung Pflegebedürftiger“ . Saarbrücken: iso-Institut ; 2005

