Nursing and Residential Care Homes
multi-disciplinary teams
Keywords: care home, hospice, palliative care, palliative geriatrics
Hospice and Palliative Care in nursing homes
Summary
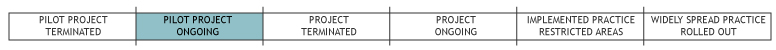
Since 2005 Hospice Austria, the umbrella organisation of about 250 hospice and palliative care organisations in Austria, has been dealing with questions concerning how to integrate hospice and palliative care in nursing homes. Hospice Austria initiated a workgroup including all relevant partners in the field to develop and define standards of quality. In 2008 the Austrian standards for hospice and palliative care in nursing homes were finalised and are now the foundation of any implementation within this project. As a pioneer, the hospice movement in Vorarlberg (one out of nine regions in Austria) started implementation of the programme in 12 model nursing homes in 2004. The region of Lower Austria started in 2009 with 8 model nursing homes and in 2010 Styria started with 6 model nursing homes. Experiences soon made clear that any successful implementation of hospice and palliative care into nursing homes needs an organisational development process as well as training for the staff. Hospice Austria initiated the development of a curriculum in Palliative Geriatrics. The aim is to enhance quality of life until the end and to enable people to die with dignity.
What is the main benefit for people in need of care and/or carers?
The ethos of hospice and palliative care includes attention to and control of pain and its symptoms, better multi-professional cooperation, better communication on all levels, more inclusion of families and loved ones into a patient’s care, and examination of ethical dilemmas. With a culture of hospice and palliative care in place all carers/professionals in nursing homes show more awareness and confidence, due to having increased their skills and professional expertise. Results of completed implementations indicate that all groups involved in the process are more satisfied: residents, families, all carers/professionals, and the management of the nursing home.
What is the main message for practice and/or policy in relation to this sub-theme?
The successful integration of hospice and palliative care improves daily communication both internally and with external groups, enhances carer/professional awareness, confidence and courage, strengthens the multi-professional team, supports dealing with difficult ethical issues, and improves the residents’ and their families’ quality of life.
It is important to develop guidelines to improve the quality of care. These guidelines aim at improving the ‘culture’ in nursing homes. The successful implementation of such guidelines in a nursing home needs a systematic approach by explaining the background of the guidelines, by initiating an organisational development process, by training staff and managers and by certification through a national authority.
The results indicate that the implementation of such guidelines makes a difference. A culture of hospice and palliative care in nursing homes enhances the quality of life for all.
Death does not need to be hidden; dying can occur with dignity. It is the task of all societies to not only to add years to life but also to care for the quality of these years.
Why was this example implemented?
For many Austrians a nursing home is their last home. Here they live - and here they die. The goal of the project ‘Hospice and Palliative Care in Nursing Homes’ is to ensure sustainable and competent hospice and palliative care in all Austrian nursing homes.
Care of older people is gaining importance as a social challenge. The symptoms of old age have changed; critical illnesses have gradually turned into chronic diseases. Many residents of nursing homes suffer from multiple terminal illnesses, which progress in phases of deterioration. This tendency implies that expertise in palliative care, palliative medicine, and palliative geriatrics is urgently required for nursing older people. Likewise a culture of palliative care should be an integral part of the processes and training schemes that make up the organisation of nursing homes. Hospice and palliative care is focussed on the residents, their families, carers, professionals, and doctors.
Description
Implementing hospice and palliative care in nursing homes started in Vorarlberg in 2004 after a survey commissioned by the federal state showed gaps in these areas. Since then Austrian guidelines (standards of quality) have been developed by Hospice Austria and a model of the necessary organisational development and the carers’/professionals’ training requirements in palliative geriatrics was issued. Experiences from (ongoing) implementations in Lower Austria and Styria are a source for constant improvement.
The following steps are recommended for the implementation process on a nursing home level:
1. Each participating nursing home appoints an authorised palliative care representative (PCR), who has attended at least one interdisciplinary basic course in palliative care and has passed a specialised training course in geriatric palliative care. The PCR will then guide and coordinate a team within the nursing home.
2. During the organisational development process the nursing home’s current practices are compared with the Austrian standards. The current practice is adapted to the standards step by step in a guided process. The process involves the management and the PCR team as well as medical doctors and an interdisciplinary team comprising the spiritual caregivers, the social workers, all kinds of therapists and the general practitioners from outside.
3. Nursing homes should create measures and structures to ensure sustainability of palliative care in the nursing home.
Working with the Austrian guidelines, a PCR’s responsibilities range from integrating them in the nursing home and having them continuously monitored and improved, to recommending additional training in palliative and geriatric care, initiating team meetings, promoting interdisciplinary cooperation, and counselling the nursing home management with regards to palliative care. The representative is always supported by his/her team.
In 2009 an Austrian advisory board for Hospice and Palliative Care in Nursing Homes was founded. It enables cooperation between Hospice Austria, the Ministry of Health and Ministry of Social Affairs, the Austrian Medical Association, the national organisation of nursing homes, the Gesundheit Österreich GmbH (Austrian Health Institute) and ÖGAM (Association of General Practitioners in Austria) and drives basic common issues forward.
The project of Hospice Austria is possible due to funding by Fonds Gesundes Österreich, a subunit of the Gesundheit Österreich GmbH (Austrian Health Institute) responsible for funding of different kinds of health promoting and practice related projects.
What are/were the effects?
A quantitative and qualitative evaluation was carried out in the first 12 model homes in Vorarlberg (2004/2005 and 2005/2006). The quantitative evaluation was a questionnaire with 26 questions answered by the director of the home and the nursing director, 20 questions by the palliative team and 4 (open) questions to the palliative care representative, director of the nursing home and nursing director. The response rate was 100%. The qualitative evaluation comprised three workshops with the palliative care team and the palliative care representative of the respective homes.
The 8 model homes in Lower Austria currently in the phase of roll out are being evaluated by the NPO Institute (Competence Centre for Non-profit Organisations located at the Vienna University of Economics and Business Administration). Results from this evaluation are due by the end of 2012.
Results of completed implementations indicate that all groups involved in the process are more satisfied: residents, relatives and families, all carers/professionals and the management of the nursing home.
Successful integration improves the daily communication both internally and with external groups, increases carers’ awareness, confidence and courage, strengthens the multidisciplinary team, helps in dealing with difficult ethical issues and improves the quality of life of the residents and their families/loved ones.
Palliative care encompasses the entire time span of a resident’s life in a nursing home - from the first day in the home until the last. Curative and palliative measures go hand in hand. From the beginning focus is put on the multi-professional assessment and management of the residents’ total pain, especially with those suffering from dementia. A resident’s quality of life (i.e. his/her best health related and personal interests) is put first when deciding medical and care related issues. Advance care planning takes into consideration situations where no doctor is available and provides guidelines for quick and effective decision making.
Family members are included in decision making and are cared for as well. Informal carers are an integral part of the team offering their services to residents and relatives alike.
What are the strengths and limitations?
The project ‘Hospice and Palliative Care in Nursing Homes’ has a positive impact on residents, their families, and professionals/carers.
Strengths
- Sustainability by combining organisational development and ongoing training, thus changing the culture of the nursing home.
- Involving all staff from cook to manager, professionals as well as informal carers.
- Commitment required by nursing home management and the home operating company as well as by federal institutions.
- The project design (architecture and guidelines) is a suggestion and open for adaptation according to varying circumstances and settings.
Weaknesses
- Although social departments of federal governments are more involved, many issues concerning nursing homes fall under the responsibility of both the social and health departments of government administration, making funding and decision making more difficult.
- Missing data with regards to achievements and services of nursing homes.
Challenges
- Providing palliative medical care and expertise.
- Getting financial support from federal institutions.
- Time commitment – nursing homes are often involved in many projects.
- Turnover rate of staff in nursing homes.
- Real multi-professional working and training all staff levels together is difficult to achieve in an hierarchical system.
- A prerequisite to achieve the objectives (i.e. contributing to the residents’ and their families’ quality of life through quality of palliative care) is the availability and presence of sufficiently qualified staff. Programmes for cutting costs in nursing homes replace qualified professionals by less qualified staff and also reduce the overall number of carers.
Credits
Author: Sigrid Beyer, Karl Bitschnau, Leena Pelttari, Anna PissarekReviewer 1: Georg Ruppe
Reviewer 2:
Verified by:
Links to other INTERLINKS practice examples
- Family Doctors contracted as staff members in care homes
- Mobile Palliative Teams (MPTs)
- Protected hospital discharge and palliative care teams
External Links and References
For more information in German and partly in English: http://www.hospiz.at/dach/HPCPH.htm
For more information on the situation in the US: Palliative care for seniors

