Policy
policies addressing continuity and mechanisms to overcome barriers at the interfaces between social and health care
Keywords: prevention, rehabilitation, England
Intermediate Care
Summary
Intermediate care services are preventive and rehabilitative services which have been nationally funded and developed over the last decade. Some services now classified as 'intermediate care' started as smaller pilot projects, but almost all health and social care communities have been working to bring these together into a more coherent and explicit intermediate care system. Intermediate care was essentially designed to prevent unnecessary hospital admissions, facilitate swift and timely hospital discharges and prevent premature admissions to permanent residential and nursing care. The term 'intermediate care' is a broad one that is used to refer to a wide range of services including rapid response, Hospital at Home, step-up and step-down care home places, supported discharge and residential/day rehabilitation. There is now a growing evidence base to help begin to understand some of the many issues that this new way of working raises. Overall the jury is still out as to whether intermediate care, although a welcome concept, will be sufficient to rebalance the current health and social care system for older people. There is evidence to suggest preventive and rehabilitative impacts for users, ease of care transitions and reduced pressure on acute services.
What is the main benefit for people in need of care and/or carers?
What is the main message for practice and/or policy in relation to this sub-theme?
Why was this example implemented?
Intermediate care was designed to reduce demand on acute services and residential care by preventing unnecessary admissions and avoiding prolonged hospital stays. These short-term yet intensive services were intended to promote faster recovery and maximise independence. Implementation of the range of intermediate care services was encouraged and supported through significant government funding and guidance. Intermediate care addresses several gaps within LTC:
- Organisational gaps. Inter-professional working is a prerequisite of Intermediate care, in particular between health/social care.
- Care sector gaps. Intermediate care focuses on avoidance or improvement of patient transition between primary/secondary care.
- National funding gaps. Intermediate care is based on a strategy to invest in community-based prevention in order to avoid expensive acute and long-term residential care.
- The focus on transition and rehabilitation at home was also intended to reduce pressure and demand on informal carers.
Although intermediate care is indeed for anyone over the age of 18, older people with LTC needs form a significant target group. In fact, intermediate care services address specific subgroups of older people e.g. services for those facing admission to residential care; rapid response to falls at home; specific dementia focus and cross over between policies as intermediate care features explicitly in the National Dementia Strategy.
Description
In July 2000 the National Health Service Plan announced around £900 million to be invested over 4 years in intermediate care services. In 2001 the government provided more detailed guidance about how intermediate care would work in practice as part of a prevention package for older people, this was updated in 2009.
Intermediate care is defined within this policy guidance as services that meet all the following criteria:
- Targeted at people who would otherwise face unnecessarily prolonged hospital stays or inappropriate admission to acute inpatient care, long term residential care, or continuing inpatient care.
- Provided on the basis of a comprehensive assessment, resulting in a structured individual care plan that involves active therapy, treatment or opportunity for recovery.
- Have a planned outcome of maximising independence and typically enabling patients/users to resume living at home.
- Time-limited, normally no longer than 6 weeks and frequently as little as 1-2 weeks or less.
- Involve cross-professional working, with a single assessment framework, single professional records and shared protocols.
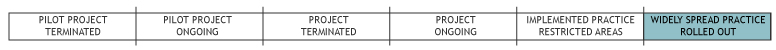
Although the development of intermediate care was nationally driven, the services have been locally designed and implemented from 2000 to present. Many services were small scale interventions which had existed prior to 2000. Other intermediate care services were newer pilot projects emerging from local partnerships to serve the intermediate care objectives.
Typical services that prevent admissions are:
- Rapid Response Teams (RRT): 24-hour rapid access service to prevent admissions for patients referred from GPs, A&E, NHS
- Hospital at Home: intensive support in the patient’s home.
Typical services that enable earlier discharge are:
- Residential Rehabilitation (Step Down & Recuperative Care): short-term therapy and enablement in a residential setting
- Supported Discharge (Community Assessment Rehabilitation Teams - CART): short-term nursing and/or therapeutic support in patient’s home
- Day Rehabilitation (Day Hospital): short-term therapeutic support at a day unit.
What are/were the effects?
National research and evaluation of intermediate care displays a high level of local variation amongst intermediate care services, making the impact of intermediate care as an overall concept difficult to assess. However, interviews with older people and their caregivers suggest that intermediate care has a significant and positive impact, providing intensive support at critical times for individuals.
A study of five English localities indicates that the development of intermediate care has led to changed working practices in service delivery and commissioning. The development of integrated care service gave clear opportunities to develop health and social care partnerships by forming joint multidisciplinary teams. Effective partnership working between health and social services organisations at both operational and strategic levels was identified as the most important lever in facilitating the development of intermediate care in local contexts. Poor partnership working, insufficient or short-term funding and workforce problems were all identified as barriers to the development of intermediate care.
The impact on organisations was seen as positive with research noting a high level of commitment and enthusiasm amongst operational staff. Impacts on the wider service system were also highlighted. Specifically, intermediate care has had an influence on mainstream practices around advocacy for patients, informing staff about alternative provision and indentifying need.
In terms of system wide changes and addressing the funding gap through investment in prevention and rehabilitation, there is not yet clear evidence that intermediate care has brought about any systemic change. However the restructuring of health and social care provision is a complex process, expected to be achieved within a longer time frame.
Of the different intermediate care services, admission avoidance schemes have demonstrated the highest level of cost-effectiveness. However, most intermediate care services are targeted towards post- acute rehabilitation rather than preventing admission.
What are the strengths and limitations?
Intermediate care displays clear potential at both individual and system level-improving patient pathway and experience and providing investment in prevention and rehabilitation to reduce demand on expensive acute or residential services. Evidence suggests that intermediate care can make a significant difference to older people’s lives – albeit that research emphasises the need to be much clearer about the groups of older people with most scope to benefit from such interventions. Another key strength of intermediate care is its ability to act as a ‘bridge’ – between locations (home/hospital and vice versa), between individual states (illness to recovery or management of chronic illness) and between sectors (acute, primary, social care and housing).
Several opportunities for development and improvement have also been highlighted.
- The need to make sure intermediate services comply with the defined guidelines and that all localities are working towards the same vision for intermediate care in practice. For instance, research highlights high levels of inappropriate referrals (e.g. not focussed on reducing use of acute/residential and services that do not deliver to the time-limited specifications.
- There is a need to move beyond the individual ‘services’ alone when developing intermediate care to concentrate on the whole health and social care system.
- Within intermediate care, provision has tended to concentrate on supported discharge, with fewer services addressing admission avoidance).
Credits
Author: Kerry AllenReviewer 1: Sabina Mak
Reviewer 2: Georgios Kagialaris
Verified by:
Links to other INTERLINKS practice examples
External Links and References
- Barton, P., Bryan, S., Glasby, J. et al (2005) A national evaluation of the costs and outcomes of intermediate care for older people. Leicester/Birmingham, Nuffield Community Care Studies Unit/Health Service Management Centre
- Department of Health (2009) Intermediate Care: halfway home. Updated Guidance for the NHS and Local Authorities
- Department of Health (2009) Living well with dementia: a National Dementia Strategy implementation plan
- Department of Health (2000) The NHS Plan: a plan for investment, a plan for reform
- Godfrey, M., Keen, J., Townsend, J. et al (2006) An evaluation of intermediate care for older people: final report. Leeds, University of Leeds.
- Kaambwa, B., Bryan, S., Barton, P. et al (2008) Costs and health outcomes of intermediate care: results from five UK case study sites, Health and Social Care in the Community, 16(6), 573-581
- Martin, G., Hewitt, G., Faulkner, T. et al (2007) The organisation, form and function of intermediate care services and systems in England: results from a national survey, Health and Social Care in the Community, 15(2), 146-154
- Regen, E., Martin, G., Glasby, J. et al (2008) Challenges, benefits and weaknesses of intermediate care: results from five UK case study sites, Health and Social Care in the Community, 16(6), 629-637

