Care from a Hospital Setting
flexible out-patient/out-reach services/ geriatric ambulatory teams
Keywords: remobilisation, out-reach services, re-hospitalisation
The Hospital comes to your Home – Outreach Geriatric Remobilisation
Summary
In order to care for the dramatically increasing number of people who need geriatric remobilisation treatment, it will be necessary to establish supplementary geriatric care facilities in addition to existing structures. Currently in Austria this type of treatment is mainly offered in departments for Geriatric Acute Care and Remobilisation, and associated day clinics.
The “Hospital comes to your Home – Outreach Geriatric Remobilisation” project has been designed to remobilise patients with multimorbidities in their own homes and to reintegrate them into society, in order to increase their self-sufficiency and reduce their need for care, thus avoiding the cycle of hospital readmissions (‘revolving door medicine’).
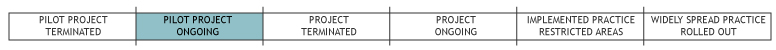
This concept is being tested in a pilot project carried out at the Elisabethinen Hospital in Klagenfurt in the district of Klagenfurt as well as in municipalities that are within a range of approximately 20 km.
What is the main benefit for people in need of care and/or carers?
Outreach Geriatric Remobilisation takes place in an environment that is familiar to patients (i.e. their home). Patients are mobilised in a place where they spend their everyday lives and therefore learn how to cope with the different obstacles they may encounter in their daily routine. In this way remobilisation is tailored to the person’s familiar housing environment and can involve the assistance of family members, friends, or carers.
This service is characterised by the following features: it takes place in everyday surroundings; patients are able to put new daily activities they have learned directly into practice; they receive support to help them become more involved in social networks; their living space is redesign; and they are encouraged to take the initiative to self-help and network. Treatment becomes part of their normal daily routine.
Patients do not have the burden of travelling to a clinic for treatment and barriers to remobilisation in the living space can be reduced. Problems are solved where they occur.
Despite some restrictions, patients are able to live an autonomous life, as the conditions of their familiar environment can be adapted to suit individual needs.
What is the main message for practice and/or policy in relation to this sub-theme?
Comprehensive outreach therapy can be offered at a significantly lower price than institutional therapy. This means considerable cost reductions for the public health sector.
Geriatric remobilisation in the home setting is able to greatly reduce or avoid the need for re-hospitalisation that is unwanted by both patients and cost-bearing units.
However, proper cooperation between all the parties of outreach and institutional health care is fundamental.
Why was this example implemented?
The concept of Outreach Geriatric Remobilisation was developed at the Elisabethinen Hospital Klagenfurt, in order to contribute to providing adequate care for the increasing number of older patients needing geriatric remobilisation. It aims to reduce re-admission to hospital and care needs and to encourage the patient to be more autonomous in their own homes.
Special attention has been paid to improving the interface between institutional, non-institutional and outreach services.
Description
Patient registration for outreach geriatric remobilisation services can basically take place in the following ways:
- Registration by the Geriatric Acute Care and Remobilisation departments for patients whose social environment permits home care and whose treatment has not finished.
- Registration by other institutions, e.g. hospitals.
- Registration by a statutory health insurance physician.
After registration, a geriatric remobilisation medical council decides whether or not a patient is suitable for the service.
The following principle applies: “As much hospital-based care as necessary – as much home care as possible.” Outpatient care takes precedence over inpatient care.
Remobilisation diagnostics take place before initiating the remobilisation programme. A complete medical history is taken and the patient is subject to a physical examination and a geriatric assessment.
On the basis of the remobilisation diagnostics, a detailed individual remobilisation plan is established for each patient.
Weekly Geriatric Remobilisation Team meetings (the complete team consists of a geriatrician, a geriatric nurse, a physiotherapist, an occupational therapist, a psychologist, a social worker, a speech therapist and one coordinator/case-manager) are intended to monitor the recovery process and, if necessary, to adapt the remobilisation plan. The contents of these meetings are documented, as well as the application of the relevant examination methods.
Care frequency and period of remobilisation:
- One therapy session with the patient takes at least 45 minutes and includes all of the therapeutic interventions performed.
- In general, remobilisation should include 40 therapy sessions.
- Therapy frequency should be at least 3 days a week.
- If needed by the individual, various remobilisation components can be applied across a longer period of time, in order to achieve the remobilisation target.
At the end of outreach geriatric remobilisation, the attending physician, the assigning institution as well as all institutions involved in further care (e.g. mobile home-care, therapists, etc.) receive a final report.
What are/were the effects?
The Outreach Geriatric Remobilisation project can contribute to reducing time spent as an inpatient, accelerate and encourage the re-integration of the patient in their familiar environment and help maintain the patient’s social network.
The programme of care of outreach geriatric remobilisation therapy is basically no different from those that take place in inpatient geriatric institutions. The only difference is that the outreach geriatric remobilisation project uses resources found inside the familiar or regular housing environment, including family/friends/carers, and especially in training and counselling them.
The project evaluation is not yet available.
What are the strengths and limitations?
Outreach Geriatric Remobilisation does not compete with existing, well functioning outpatient or outreach care services. Instead, it represents a valuable contribution to improving the link between institutional and non-institutional services.
What is important is that all forms of outreach therapy take place only in cooperation with and after consultation with the patient’s GP. They must be involved in all activities from the beginning. The GP's duties (home visits, issuing prescriptions, etc.) are unaffected by the programme. The geriatric team does not provide basic care.
Strengths
The entire geriatric team is available and provides the same therapies as inpatient treatment but with major advantages, since the therapies take place in the patient's private home.
While achieving the same level of performance, outreach therapy is available at a much better cost then institutional treatment. Outreach therapy is more efficient and more sustainable.
Each euro that is invested in this project pays off in multiple ways. Valuable resources can be saved as less time is spent on mobile home-care, in admission to a nursing home or hospital, and through the prevention of further ill health, such as falls.
Potential weaknesses
It is challenging to establish cooperation with the practice-based GPs, therapists and mobile home-care service providers. This is a decisive factor, since the practical implementation of this concept should demonstrate that open and direct communication and cooperation between intra- and extramural care establishes an interface from which patients, their families and all parties involved can benefit.
Opportunities
The concept of outreach geriatric remobilisation can be integrated in all geriatric departments and thus represents a valuable contribution to inter-connected geriatric services and helps to increase the attendance of multi-morbid patients.
Possible threats
The funding application for the ‘Reform Pool Project’ (projects which intend to foster cooperation between institutional and non-institutional care in Austrian regions) was submitted on 27 April 2009. The project was comprehensively discussed by a task force comprising representatives of the federal governments, the public health insurance agency and the applicant and was unanimously considered valuable. However, due to some small issues the health platform has not yet released the project funding.
Credits
Author: OA Dr. Walter MüllerReviewer 1: Georg Ruppe
Reviewer 2: Laura Holdsworth
Verified by:
External Links and References
- A.ö. Krankenhaus der Elisabethinen Klagenfurt GmbH
- ÖGGG (Österreichische Gesellschaft für Geriatrie & Gerontologie)
- Todd C, Skelton D. (2004) What are the main risk factors for falls among older people and what are the most effective interventions to prevent these falls? Copenhagen: WHO Regional Office for Europe (Health Evidence Network report).
- American Geriatrics Society; British Geriatrics Society and American Academy of Orthopaedic Surgeons Panel on Falls Prevention (2001) 'Guideline for the prevention of falls in older persons' in: Journal of the American Geriatrics Society, Vol. 49: 664-72.

