Care from a Hospital Setting
structures that facilitate integrated discharge and follow-up planning
Keywords: hospital discharge, delayed discharge, multidisciplinary
Hospital discharge unit/lounge
Summary
Discharge lounges/units are areas of the hospital where patients who have a planned discharge arranged can be transferred to complete the discharge process. The various activities that can take place in discharge lounges include: meeting transportation, receiving prescription medication from the pharmacy, and completing discharge paperwork. More comprehensive discharge units may also include beds for patients to use, shower facilities, have nursing staff available at all times, and a very few are open 24/7.
What is the main benefit for people in need of care and/or carers?
Discharge units have the potential to discharge patients at any time of day, any day of the week or could be used as a holding area if the patient is to be transferred into a care home. Transportation can therefore be arranged at a time of day suitable to the patient or on a weekend, rather than being rushed on a Friday prior to the weekend.
What is the main message for practice and/or policy in relation to this sub-theme?
The concept of the lounge was developed in order to free up acute beds quicker for incoming patients (i.e. reduce ‘bed-blocking’). Discharge lounges are increasingly being used across hospitals in England to meet government policy on delayed discharges and have links to Intermediate Care.
Why was this example implemented?
Discharge from hospital is a complex process which requires the coordination of multiple disciplines and care providers. Because of this complexity there are often delays in discharge and transfer on the planned discharge day despite planning for discharge early on in the patient’s admission to hospital. Any delays in transfer can result in the following problems (NAO, 2000) which are costly and detrimental to the care of other patients:
- ‘Bed blocking’ as peaks in admissions occur earlier in the day than when discharge occurs
- Increased waiting times in A&E departments
- Medical patients being placed in surgical beds.
Discharge lounges/units can help bridge the gap between acute admission and return to the community and also expedite the intake of new admissions as beds are freed up. All patients can be transferred to the discharge lounge, not just older people.
Description
The discharge lounge generally includes only chairs as a waiting area and may only be available at certain times of the day and with lower grades of staff available (e.g. HCAs). More comprehensive discharge units may also include beds for patients to use, shower facilities, and have nursing staff available at all times. Very few units are also open 24 hours a day, seven days a week. Such units have the potential to discharge patients at any time of day, any day of the week or could be used as a holding area if the patient is to be transferred into a care home (see example on Intermediate Care). Discharge units may also have a number of dedicated staff for facilitating discharge from hospital, such as occupational therapists who can complete home visits and have links in the community. Specific processes which can be sped up by the discharge unit are: meeting transport (family, friends, or transport services), receiving medication from the pharmacy, and completing discharge paperwork or electronic discharge. The discharge unit requires space in the hospital as any other unit or ward would. Specialised discharge coordinators can also be a part of the unit and begin planning for the patient’s discharge on admission.
The Discharge Unit at West Suffolk Hospital is an example of a comprehensive unit. It is open 24 hours a day, seven days a week for those with a planned discharge within 24 hours and provides qualified nursing support throughout this period. Beds, telephone, toilet and shower facilities are available and hot meals can be provided as would be on the ward. Medication and discharge arrangements can be discussed by a qualified nurse staffed in the unit. Patients can stay in the unit until their transportation arrives.
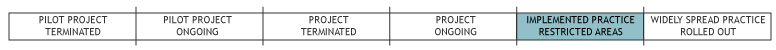
Discharge lounges are supported by the Department of Health to help streamline the process on the day of discharge and are suggested as a good practice example in its guidance on hospital discharge (HSCJU & CAT, 2003). They have been in use for over 10 years. Implementation of the discharge lounge or unit varies by hospital, though there seems to be an increasing move towards the more comprehensive unit type as illustrated by the West Suffolk Hospital example.
What are/were the effects?
There is evidence that discharge lounges/units have had the following positive affects (NAO, 2000):
- allow beds to be freed sooner therefore increasing capacity
- help ease the collection of patients for transport
- help in the delivery of medication to patients to take home.
However, they can also lead to increased workload on ward nursing staff as wards are able to take more patients as beds become available faster.
The overall impact on LTC as a whole is likely limited as its effects are largely focussed on streamlining hospital processes and whether its benefits are felt by social services is unknown. Integration of discharge lounges/units varies by local implantation and not all hospitals are using them. However, the number of discharge lounges/units in use is growing which likely indicates its potential for mainstreaming and sustainability.
What are the strengths and limitations?
Strengths
- Discharge units function in the reverse way as admission units and therefore should be easily transferable across countries and systems. They do not require any set preconditions, though electronic systems in hospital would be preferable.
- Discharge lounges help streamline processes on the day of discharge – essentially the transition from acute care to community care. Discharge lounges allow resources to be freed up for new admissions thus reducing waiting times for incoming patients.
Weaknesses
- The discharge lounge/unit is only effective as part of a holistic discharge policy and requires many steps to be taken prior to internal transfer to the discharge unit.
Opportunities
- Discharge units should be seen as more than just a waiting area, which in some more basic implementations is all that lounges are. Having a discharge unit available 24 hours a day 7 days a week could allow patients to be discharged at any time of day any day of the week. This concept would also increase the benefit to patients as they could potentially go home at weekends or at night when they are ready as currently the benefit of lounges is primarily concerned with streamlining resource allocation in hospital.
Threats
- Discharge units could be threatened as any other hospital department might, though all patients inevitably need to be discharged so therefore their function is always needed especially as they save costs.
Credits
Author: Laura HoldsworthReviewer 1: Barbara Weigl
Reviewer 2: Lydia Brichtova
Verified by:
Links to other INTERLINKS practice examples
External Links and References
- Bird J. (2008) ‘Discharge made simple’. Nusingtimes.net [Online] http://www.nursingtimes.net/discharge-made-simple/1477936.article
- Department of Health - Discharge from hospital pathway, process and practice
- National Audit Office (2000) Inpatient admissions and bed management in NHS acute hospitals. London:TSO.
- West Suffolk Hospital (2004) Your guide to the discharge unit.
- Health & Social Care Joint Unit and Change Agents Team (2003) Discharge from hospital: pathway, process and practice. London: DH. (Good practice guidance)
- Nursing Care Journals and Blog

