Interdisciplinary work
fostering a culture of collaboration (requirements, training, team building)
Keywords: joint working, prevention, community care
Partnerships for older people projects (POPPs)
Summary
The Partnership for Older People Projects (POPPs) was funded by the Department of Health to develop services for older people. The services were specifically aimed at promoting health, well‐being and independence and preventing or delaying their need for higher intensity or institutional care. Twenty‐nine localities across the country were involved as pilot sites. Partnership working was essential component of POPPs methodology and local authorities worked with health and third sector partners to develop and deliver services. All local projects also involved older people in their design and management.
The projects offered an opportunity for local partners (including the older people themselves) to strengthen and improve their relationships and knowledge of services. These partnerships demonstrated results of increased referrals as local knowledge grew and the development of a range of LTC services, from low level measures in the community to formal preventative initiatives such as co-ordinated case identification and management. The example draws on national and local evaluation to explore the potential of such funding programmes to foster sustainable inter-organisational co-operation and increased user involvement in LTC services. It also examines direct outcomes for services users and local health system efficiencies and savings.
What is the main benefit for people in need of care and/or carers?
This programme of partnership focused projects for older people provided opportunities for the development of local services. Evaluations demonstrated a high level of user participation in service design and governance, as well as increases in quality of life outcomes for service users.
What is the main message for practice and/or policy in relation to this sub-theme?
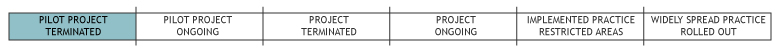
In general the POPPs programme led to improvements in local partnership working and service user outcomes. Although the majority of funded activities have been mainstreamed, the ‘pilot’, time-limited nature of the funding leaves the services vulnerable to funding cuts.
Why was this example implemented?
The primary objective of POPPs was to improve the health and wellbeing of older people through the work of local projects. The projects focused on supporting a wide range of older people in the community through health promotion and other integrated health and wellbeing services.
POPPs had a clear intention of improving local interfaces and strengthening local networks; between organisations and actors, across health and social care, between different sectors, as well as service users.
The example explores some of the key initiatives carried out as part of POPPs and their success, impact and learning.
Description
29 pilot sites (led by local authorities) for projects were funded by the Department of Health, with total funding of £60 million (€70.5). The sites were funded in two rounds between 2006 and 2009. From the 29 sites 146 core projects were set up to respond to local priorities. Two thirds focused on the community, addressing social isolation and/or health promotion. One third focussed on reducing pressure on acute care, decreasing admissions and improving hospital discharge. Examples of interventions within projects are:
- Training programmes for health and social care staff in older people’s services
- Web-based information services
- Handyperson schemes
- Befriending schemes
- Welfare advise and signposting services
- Holistic assessments
- Falls prevention
- Carer support
- Rapid response teams
- Case management
- Case finding initiatives
For further details and examples of the various activities undertaken within POPPs and the composition of the teams implementing these, please see the national evaluation- final report.
522 organisations were involved alongside local Councils as partners within the projects including: Health trusts; emergency services; housing associations; voluntary organisations; private sector organisations.
Service users’ average age was 75 and two thirds were women. 81% of the total 264,000 service users lived in their own homes, others lived in residential or sheltered accommodation.
The POPPS initiative was shaped by the 29 local authorities and partners responding to the Department of Health funding opportunity. The locally tailored designs were allocated varying budgets e.g. Leeds £4,046,000; Luton £861,000; Manchester £2, 601,000.
Notable characteristics of POPPs were: mandatory ongoing service testing and evaluation; and involvement of service users in design, recruitment, governance, provision and evaluation. User involvement took the form of advisory panels, workshop planning/decision-making events, staff interviews/selection panel membership, as voluntary or salaried service provision staff, as evaluators or interviewees in evaluation.
What are/were the effects?
As well as ongoing local evaluations the Department of Health commissioned a national evaluation of the Programme, undertaken by Personal Social Services Research Unit (Universities of Kent and London School of Economics).
The national evaluation found that the impact on joint working was positive. This was found especially where multi-agency staff worked together in one location, rather than in virtual teams. Better referrals across agencies, beyond POPPs services, were a linked benefit of improved partnership working.
User involvement was a strong outcome of the POPPs projects. 77% of projects involved users in service design and 93% included users or carers on governance boards and steering committees.
Quality of life for participants/users of various POPPs projects was measured against a control group of older people with no participation, using EQ-5D health related quality of life measures. Significant increases in quality of life (12%) were found in POPPs projects providing exercise and practical help. Smaller increases (3-4%) were found in case co-ordination and falls prevention focused projects (Windle et al. 2010: ix-x).
The impact of information and advice work was seen through increased receipt of state benefit. The overall annual increase in benefits claimed was £53,768 (€62,500), claimed as personal care support (attendance allowance).
Cost reductions and efficiency of services were suggested to be significantly improved in comparison with non-POPPs sites. There are also indications that POPP pilot sites have an effect on emergency hospital bed-days use. The results show that for every £1 (€1.16) spent on POPPs, an average of £0.73 (€0.84) will be saved on the per month cost of emergency hospital bed-days.
85% of POPPs projects gained funding to sustain their project activities beyond the government funding programme, most funding came from local health Trusts. Only 3% of projects closed down. Further incentives to fund POPPs activities came from the social care ‘transformation agenda’, presented in the 2006 White paper ‘Our Health, our care, our say’. The agenda incorporated a similar focus to POPPS around person-centres approaches and integrated services, encouraging investment from health authorities. Evidence from local evaluations was also a key incentive for investment.
What are the strengths and limitations?
Many of the benefits of the POPPs programme relate specifically to improved working structures and practices of the service provider organisations (for further detail see the national evaluation- final report):
- More systematic, evidence-based and ‘joined-up’ systems for making commissioning decisions in local areas. These systems were the result of either specific ‘case finding initiatives’ or other joint work and shared local knowledge of service users and services achieved through POPPs activities
- Making more effective use of a wide range of resources, services and skills available in the voluntary sector, resulting in a more mixed economy of service provision to support local older people
- New systems for referral and sharing of information have been established through POPPs, which have improved the way in which different services work together
- POPPs has reinvigorated locality working with local older people to identify needs and inform commissioning processes not only for health and social care services, but also for wider well-being services (Windle et al., 2008).
However, as initially time-limited and localised pilot exercises, the impact of the POPPs programme is to some extent limited. Although measures were built into the programme in an attempt to ensure the sustainability of positive outcomes, evaluators identified several factors which may impede the mainstreaming process as it progresses, including financial constraints; inability to attribute positive gains to particular interventions; and changes in government policy.
However, despite these difficulties the vast majority of services developed within POPPs projects have been sustained beyond the timeframe of the central government funding. Such services are currently supported financially by local health authorities.
Major reform including the abolishion of Primary Care Trusts (who currently fund ex-POPPs project activities) could be a potential barrier to the sustainability of these interventions.
Credits
Author: Kerry Allen, University of BirminghamReviewer 1: Stephanie Carretero, University of Valencia
Reviewer 2: Ricardo Rodrigues, European Centre for Social Welfare Policy and Research
Verified by:
Links to other INTERLINKS practice examples
External Links and References
- Department of Health (2006) ‘Our health, our care our say’.
- Windle, K., Wagland, R., Forder, J., D’Amico, F., Janssen, D. and Wistow, G. (2010) National Evaluation of Partnership for Older People Projects: Final Report. Kent, PSSRU.

