Values
how values relating to prevention and rehabilitation are considered
Keywords: integrated care, clinical continuity, home care, patient centred, chronic illness
Clinical continuity by integrated care
Summary
HOMECARE is a European collaborative project funded by the EU 7th Framework Programme. This example describes the major outcome of this project, which is the implementation of Integrated Homecare (IHC). IHC has been developed in response to the call for better clinical continuity in the treatment of chronic conditions as set out by the WHO Europe Office 2002. Our initial systematic review (Larsen, 2011) of research in integrated care concludes that examples of IHC for patients with stroke, Chronic Obstructive Pulmonary Disease (COPD) or Heart Failure (HF) are the most promising to take forward. IHC has been implemented at a regional level where the clinical and administrative levels are able to negotiate directly to shape IHC services in accordance with local conditions.
The key message is that IHC represents a potential WIN-WIN-situation for citizens who are both patients seeking the most effective care, and tax payers/those paying insurance seeking the best value for money. Against this background the real challenge of IHC is to improve organisation of health care with scarce finances whilst still upholding the set of values.
What is the main benefit for people in need of care and/or carers?
- IHC takes place in the home of the patient as part of an integrated care pathway between hospital services, primary care and social services for patients with specialised care and individualised rehabilitation needs, so that central to its value system is a person-centred approach.
- The IHC-team focuses on effectiveness, quality, access and user satisfaction in an economic way and uses tele-facilities where they can support these goals.
What is the main message for practice and/or policy in relation to this sub-theme?
By providing a flexible service that fits to local needs, IHC has developed an effective locally disseminated strategy and service that lies outside of central control. This strategy focuses on European regions and is able to negotiate and shape the way that clinical and administrative services can work together and share the same values.
Warum wurde diese Initiative implementiert?
IHC is implemented with the dual purpose of reducing poor outcomes as well as length of stay (LoS) for large groups of patients with chronic conditions. For stroke patients poor outcomes are defined as the aggregate of deaths and referrals to nursing homes at 6 months follow-up which in usual care amounts to 25-35%. For patients with HF or COPD poor outcomes are represented by high frequencies of readmission to hospital. The gap between hospital care and primary care/social services in particular seems to be a key factor that needs to be overcome to reduce these high outcome levels. IHC therefore has the potential to cut poor outcomes for these groups by 33-50%. A particular factor in the efficacy of IHC stems from the finding that blood pressure reduces by 5-7 mmHg when part of the patient’s rehabilitation is transferred from a clinic to the home setting. This reduction brought about by providing a more relaxed environment improves cognitive function, which in turn benefits the efficacy of rehabilitation (Larsen, 2010). Alongside this measurable outcome, the value base of IHC enables a more individualised rehabilitation based on a better knowledge of the habits and preferences of the patient. For example, following a stroke, a patient who has previously enjoyed cycling can continue, following adaptations to their bicycles.
The shortening of LoS may be seen as a new phase in the continued improvement of hospital productivity. Since the 1960’s LoS has been considerably shortened by the introduction of out-patient facilities for both pre-investigation and post-discharge follow-up. To continue these improvements, hospital at home services such as IHC seem to be relevant.
Beschreibung
Partners define Integrated Homecare (IHC) as a specifically patient-centred care (Kodner, 2009):
- IHC takes place in the home of the patient as part of an integrated care pathway between hospital services, primary care and social services for patients with specialised care and individualised rehabilitation needs.
- The IHC-pathway should be financially and administratively coordinated with a view to effectiveness and savings on stationary resources in health care and/or social services.
- IHC is performed by a multidisciplinary team in collaboration with the patient in the home of the patient as well as in the hospital, passing eventual general care needs to the community care setting.
- The IHC-team focuses on effectiveness, quality, access and user satisfaction in an economic way and uses Tele-facilities as far as they serve these goals.
By this definition IHC is supposed to support rehabilitation values of Psychology (Servellen et al, 2006) as:
- Perceived control over their care (feeling safe)
- Greater involvement in decision-making (participation)
- Knowledge about their illness and its treatment (health information/education)
Searching for evidence of efficacy, a systematic literature review identified stroke, COPD and HF as the most obvious prototypes for IHC. A characteristic of IHC is that groups of health professionals such as therapists and nurses rather than physicians have to reorientate their practice. So, most home sessions in IHC Stroke are done by a outreach team of therapists from the hospital. IHC COPD and HF both have a community-based nurse as ‘case manager’.
In principle there should not be severe financial difficulties with IHC as it is expected to give societal net savings. However, restricted cash-flow situations can be a barrier to implementation. A hospital for example may have a net cost providing IHC stroke services while the community authorities get most of the benefit, eg. through reduced need of permanent nursing homes. Conversely, for IHC COPD and HF, community nurses contribute to the service while the hospital receives the benefit of reduced readmission. Such financial barriers have to be overcome as part of the implementation strategy.
Welche Effekte wurden erzielt?
Within the EU HOMECARE partnership, the framework being used for comprehensive evaluation of IHC is health technology assessment (HTA). This means that aspects of safety, clinical effectiveness, patient’s experiences, economics, organisation and socio-culture/ethics/legality are being included and analysed. From an overall EU perspective the analysis to date is indicating the following broad effects:
- IHC Stroke shows a significant reduction of long term need for help/nursing at home. Net savings per patient are calculated to €2,000, with a worst case of €1,000.
- IHC HF and COPD combine significant reduction of readmissions with net savings of about €500 and €1,500 per patient, respectively.
- In all, IHC is a cost-effective form of secondary prevention relevant to about 1.5 million new patients per year in EU27 with an expected average net saving of €1,700 per patient.
- By providing a flexible service that fits local needs, IHC has developed an effective locally disseminated strategy and service that lies outside of central control. This strategy focuses on European regions and is able to negotiate and shape the way that clinical and administrative services can work together and share the same values.
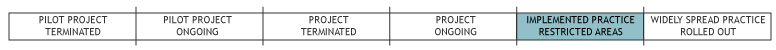
Out of the three focused variants of IHC, IHC Stroke is the most widely researched. About 15 good RCT studies have been published and from these two have been done by HOMECARE in Denmark and Portugal. IHC Stroke has been established in increasing numbers in Scandinavia and the UK. In Europe, heart failure management programmes including homecare elements, exist in about 40% of all heart clinics. Documented cost-effective IHC HF–programmes are reported in Spain, Greece and Germany. Regarding IHC COPD, cost-effective programmes are reported from Spain/Belgium and Ireland.
A number of promising trials are actually running in more countries in all 3 variants of IHC, some financed by the EU.
Worin bestehen die Stärken und Schwächen der Initiative?
A comprehensive analysis of the relative Strengths, Weaknesses, Opportunities and Threats (SWOT analysis) regarding IHC is shown below. While the section above provided an EU perspective, the SWOT has been done from the perspective of the local project planning/operational stage. It serves to give an impression of the issues that came to the fore in order to produce the best possible design of IHC. For the sake of simplicity only the three most important aspects of each of the dimensions are described:
Strengths
- Dominant interventions (Both beneficial to patients and economic to providers) creating synergy
- Based on a holistic approach shared by more health professions
- Job enrichment to therapists and nurses
Opportunities
- Potential benefits for a majority of people to be accelerated by a further follow-on project in development (Homecare2)
- Low-Tech interventions provide a feasible approach in countries with fewer financial resources
- General improvement of organisational quality
Weaknesses
- Lack of trust across the secondary/primary interface
- Relative low medical research priority
- Moderate improvements on a day-to-day base
Threats
- Fragmented financial conditions
- Mono-disciplinary strategies
- Mediocre implementations without effect
In summary, weaknesses/barriers and threats seem relatively severe compared to the strengths and greater dissemination efforts are required beyond a ‘HTA of IHC in EU’. The gap between theoretical opportunities and practical barriers may be bridged focusing on the formation of as many implementation projects as possible. Professionals tend to respond much more positively to ‘real-world-implementation’ by their peers than to a scientific HTA.
Impressum
Autor: Torben Larsen, CAST, University of Southern Denmark, OdenseReviewer 1: Kim Hørslev-Petersen
Reviewer 2: Bibi Hølge-Hazelton
Verified by:
Externe Links und Literatur
- Kodner, D (2009) 'All ToGETHER Now: A Conceptual Exploration of Integrated Care' in: Healthcare Quart, Vol 13, Spec. Issue.
- Larsen, T (2010) 'Neuroeconomics and Public Health' in: Acta Systemica, No 1.
- Larsen, T (2011) 'Clinical Continuity by Integrated Care', pp. 241-61 in: M Guah (Ed) Healthcare Delivery Reform and New Technologies: Organizational Initiatives. Hershay: Idea Group Publishing.
- Servellen, G, Fongwa, M & EM Errico (2006) 'Continuity of care and quality care outcomes for people experiencing chronic conditions: A literature review' in: Nurs Health Sc., Vol. 8: 185-195.
- The HOMECARE website informs on all aspects of IHC: www.integratedhomecare.eu

