Formal Care in the Home and Community
structures that facilitate coordination and cooperation with other formal and/or informal care
Keywords: hospital patient, cross-sector coordination, follow-up home visits, readmission, co-financing
Follow-up home visits after discharge from hospital
Summary
Follow-up home visits after discharge from hospital for people aged 65+ in a Copenhagen local authority started in 2007 to reduce re-admissions and strengthen the cross-sectoral coordination of services. From the very beginning an essential element of this reform was the joint working between regions, local authorities and GPs. The reform led to local authorities having to co-finance all hospital admissions, though with a ceiling per individual patient at 30%. Follow-up home visits from health care services were one in a series of initiatives that were taken to ensure cohesive patient treatment and care as well as simplified access to prevention, examination, treatment and care.
The project was evaluated in 2010. Two qualitative focus group interviews showed that the involved health care staff generally have a positive approach and interest to optimise the process concerning follow-up home visits so that citizens can benefit fully from this initiative.
A second evaluation (quantitative) to monitor and analyze the costs of the intervention will take place in 2011.
What is the main benefit for people in need of care and/or carers?
The main benefits were to optimize the process concerning follow-up home visits after hospitalisation, so that citizens can benefit fully from this form of follow-up initiative.
What is the main message for practice and/or policy in relation to this sub-theme?
The reform led to local authorities having to co-finance all hospital admissions, though with a ceiling per individual patient at 30%.
Warum wurde diese Initiative implementiert?
Research shows that the risk of re-admission of discharged vulnerable older patients is high. By preventable re-admission it is understood that a patient returns to the hospital as an inpatient for further treatment, although improved follow-up after original discharge could have prevented this event.
In 2003-2005 a randomised, controlled intervention study of follow-up home visits by GPs and home nurses showed that the number of re-admissions was reduced. Admissions for the control group were 52% and for the intervention group 40%. A saving per patient of €670 was calculated.
Based on this evidence, in November 2007 the local authority opened 12 acute beds in a home for older people as a first new initiative against re-admissions, administrated by the health care service. This initiative meant that, instead of hospitalisation, older people could get treatment in acute beds provided in the municipality. Local authorities that in Denmark, have to co-finance (30%) all hospital admissions – though with a ceiling of approximately €600 regardless of length of stay – saw this as a way to save money. However, it is important to emphasise that this mechanism is a necessary tool to incentivise improvements and gains in efficiency.
The gap addressed by this example specifically concerns unnecessary hospital re-admissions of older people, i.e. admissions that could have been prevented with systematic and co-ordinated follow-up after original discharge and/or general prevention activities. The example aims to highlight the value of home visits as a useful preventive initiative and shows solutions to overcome gaps at the interface between hospital and home care.
Beschreibung
The purpose of the reform has been to strengthen the organisation of home visits and the co-ordination between the health care staff by means of a direct contact by telephone or e-mail between hospital doctors and GPs before the discharge of a patient.
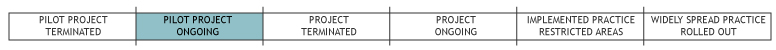
The project is being conducted as a randomised controlled investigation and is to test and further develop follow-up home visits after hospital discharge. If the investigation shows that the measure has a positive effect, the intention is to offer this form of follow-up initiative to all hospital patients in Copenhagen. A follow-up home visit generally means a home visit within about one week after discharge from hospital by a general practitioner (GP) and a district nurse. This home visit can be supplemented with two subsequent visits/contacts in the home of the patient or with a GP if this is considered necessary. Such additional visits/contacts have to take place at three and eight weeks after discharge.
The financial resources for the entire project come from a medical technology evaluation (MTV) budget of the local authority.
The pilot project was completed in March 2011. It covered three localities within the Copenhagen local authority area, with a total population of 149,358 (2007 figures), of which the 75+ age group makes up 9,077 citizens. (The age group was extended to 65+ but no figure for total citizens was given.)
Welche Effekte wurden erzielt?
An evaluation in 2007 shed light on the organisational challenges in relation to the successful implementation of follow-up home visits. The evaluation is based on a qualitative investigation of the most central players in the area. One focus group interview has been conducted with project employees (doctors and nurses) who have been involved in the project on follow-up home visits. Another focus group interview has been conducted with district nurses who were involved in the project. Two individual interviews were held with employees from home care services in the City of Copenhagen and five individual interviews were held with GPs who have been involved in the project.
The main challenge identified by the participants in the evaluation concerned simplifying and clarifying how the follow-up visits for the parties involved were organised. This required, for example, facilitating and improving communication and the flow of information from one party to another. The main challenges were
- to create a more efficient transfer of patient information, including specifically discharge letters (summaries of patient records) and medicine lists
- to create a simpler flow of communication in relation to agreements on follow-up home visits, e.g. through direct contact between the hospital and GPs when patients are discharged
- to clarify the benefits of follow-up home visits compared to other types of follow-up schemes for the same target group, e.g. ‘accompany home’ schemes that are currently being initiated at hospitals in the Capital Region of Denmark
A main future challenge will be to involve the hospital wards more closely in the process of offering follow-up visits. The hospital wards should become more responsible for assessing whether a follow-up home visit is a suitable follow-up initiative for the patient in question. In general practice, the challenge is mainly to get the GPs to participate more actively in follow-up home visits.
Worin bestehen die Stärken und Schwächen der Initiative?
Strengths
- The pilot project has undergone a qualitative evaluation that showed a generally positive effect of the follow-up home visits by all staff groups involved.
Weaknesses
- A cost effectiveness evaluation will take place by mid 2011.
- The elderly persons aged 65+ have not yet been asked about their opinion.
Impressum
Autor: Lis WagnerReviewer 1: Laura Holdsworth
Reviewer 2: Laura Cordero
Verified by:
Externe Links und Literatur
- Hjelmar, Ulf (2010) A quantitative evaluation of the organisation of follow–up home visits in Copenhagen local authority. Copenhagen: AKF.

