Formal Care in the Home and Community
flexible and adaptable services to suit individual needs and individual lifestyle
Keywords: palliative care, multi-professional team, mobile services, terminal illness, preferred place of care
Mobile Palliative Teams (MPTs)
Summary
Since 2000 a total of 36 Mobile Palliative Teams (MPTs) have been established and implemented in all Austrian provinces according to a national plan for graded hospice and palliative care. This national policy was combined with the intention to reduce unnecessary hospitalisation and to cope with a growing number of potential clients. These were the main drivers for the development and continuous expansion of MPTs in Austria.Services delivered by MPTs can be taken up by clients with chronic and terminal illnesses living at home as well as by professionals, who work in mobile or residential LTC services and need support with issues of palliative care or treatment. Composed of a multi-professional group (always consisting of medical doctors, nurses, physio-, psycho-, speech- and occupational therapists as well as dieticians and pastors) an MPT collaborates and coordinates interventions with the client’s existing formal and informal network. In 2010 it was estimated that one MPT was needed for every 140,000 inhabitants (approx. 57 MPTs) in Austria. The national umbrella organisation Hospiz Österreich monitors the development and current expansion of all related services.
What is the main benefit for people in need of care and/or carers?
Registered clients of MPTs and their caregivers benefit from individually adapted plans for home visits including all kinds of specific services provided by the multi-professional teams. Telephone counselling and acute (medical) care are available over a 24 hour period. Additionally, support to coordinate admission to or discharge from hospitals as well as transfer to hospices is offered by MPTs.
What is the main message for practice and/or policy in relation to this sub-theme?
MPTs represent a promising role model for mobile community care services for frail older people in general. The multi-professional composition of MPTs as well as the individuality and flexibility of provided services appear as important success factors.
Warum wurde diese Initiative implementiert?
In 2000 palliative medicine was mentioned and introduced for the first time in the Austrian Krankenanstalten und Großgeräteplan ÖKAP/GGP (see ÖBIG 2004), which means a plan that determines the general structural requirements of hospitals and the national acquisition and distribution of large and very expensive health care related machines, such as computer tomographers or other special machines. Since then there has been systematic planning and development of structures and respective quality criteria necessary for Hospice and Palliative Care in Austria. The scheduled implementation of a graded Hospice and Palliative Care system containing different forms of inpatient and outpatient services has been compiled in the respective national plan Abgestufte Hospiz- und Palliativversorgung in Österreich (ÖBIG 2004). Mobile Palliative Teams (MPTs) represent one essential component of this implementation plan.
The main target group of Mobile Palliative Teams are people with chronic and terminal illnesses living at home (not in particular frail older people). MPT services can also be taken up by professionals (family doctors, medical and nursing staff in the LTC sector) in need of support with issues of palliative care and treatment. Services by MPTs are also accessible for socially disadvantaged people.
The underlying intention and general objective of MPTs is the provision of multi-professional and continuous mobile palliative and social care in order to maintain or improve quality of life and to allow a terminally ill person to stay at home and/or in familiar surroundings as long as possible and to avoid (unnecessary) hospitalisation. Another important objective is to bridge common gaps and facilitate transition processes between hospital and (nursing-) home care, which can be exhausting and sometimes even traumatising for a terminally ill person.
Beschreibung
Clients or their carers, who directly want to take up services by MPTs, have to register in advance with a respective regional provider organisation. They often do so on their own initiative or after having received preliminary information about such services, e.g. by their general practitioner. After an initial home visit, where specific needs and circumstances of the client are assessed, an individual care and support plan is set up in coordination with the user, carer and with other professional staff already attending the client, such as general practitioners or home care providers. There are a number of things that will be determined in the care plan; these include the frequency of home visits, the appropriate kind of palliative care and treatment as well as relevant additional services, such as psychosocial support, occupational therapy or assistance by volunteers. Over the course of time the individual care plan will be continuously adapted to meet predominant and current needs of the client. Mobile medical services and telephone counselling are available 24 hours a day.
Services by MPTs may also be provided as support service to medical or nursing staff in LTC institutions. Mobile palliative care in Austria is generally free of charge for the client. Services are mainly financed by sponsoring, private donations, and public funding. Apart from a basic salary, providers (mainly non-profit organisations) usually pay their staff according to their time on duty (e.g. time spent for a home visit) and not according to specific kinds of interventions performed (e.g. to administer an injection). This has an obviously significant positive influence on the general quality of services. Staff members of MPTs can be solely employed by the respective provider or work part time with the MPT and have an alternative work (e.g. in a hospital or in individual practice).
The Austrian Federal Institute for Health Quality has determined criteria for the establishment of MPTs (ÖBIG 2004). Apart from 24-hour availability for telephone counselling and for acute (medical) interventions, the service provision by a multi-professional team is a basic requirement. Medical and nursing staff, at least one social worker and administrative staff, have to be present in a MPT. Additionally, physio-, psycho-, speech- and occupational therapists as well as dieticians, pastors from different confessions and volunteer workers have to be available to each team. Most providers of MPTs also collaborate with teams of hospice volunteers, who have to pass a basic course in palliative care and engage mainly in home visits and supportive activities.
Welche Effekte wurden erzielt?
MPTs facilitate the transition process between hospital and home care and seek to coordinate their activities with existing professional and private networks (family doctor and medical specialists, mobile-/24-hours care staff, family members etc). In this way valuable links to family members as well as to health and care professionals already involved in care are usually established. To support a person in their desire to stay at home and/or in a familiar surrounding as long as possible can positively influence clients’ subjective feelings concerning independency, autonomy, and health. Costs for the user and in particular for the public health care sector can be assumed to be generally lower compared to care in hospitals or other institutions. A cost analysis and evaluation report from 2008 on Mobile Palliative Teams in the city of Graz (region of Styria) shows that in particular hospital related costs for terminally ill patients in the last month of life could be reduced significantly by interventions of MPTs. While services by MPTs accounted for average costs of €729 per client in the last month of life, average hospital related costs could be reduced from €5,855 to €3,523 for this same period (Joanneum Research, 2008). A recent study from the US widely confirms these results.
Additionally, having multi-professional support and advice available 24 hours a day is of great relief for a carer. Psychosocial support is usually offered to caring family members by MPTs. However, the physical burden and amount of necessary care work at home cannot be reduced significantly by MPTs alone.In general MPTs have been established to support and take care of terminally ill people (often oncologic patients) in their private environment. However, this type of multi-professional care and treatment also seems to be a very attractive idea for providing palliative care to frail older people, who want to die at home. In this way MPTs do not only foster multi-professional cooperation within their specific domain, but might also impact on future LTC concepts for frail older people living at home or in nursing homes. Currently MPTs exist in all Austrian provinces in slightly varying prevalence and organisational forms and further expansion is to be expected. An annual survey monitoring the development and delivery of hospice and palliative care services in Austria according to the guidelines of the plan Abgestufte Hospiz- und Palliativversorgung in Österreich (ÖBIG 2004) is undertaken by the Dachverband Hospiz Österreich.
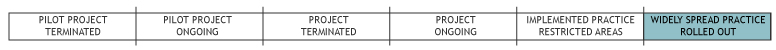
According to the last available survey a total of 36 Mobile Palliative Teams had been established all over Austria by 2010 – five more than in 2007 – and 7,757 clients had been taken care of by Palliative Care Teams over 2010 (Pelttari et al., 2011). For 2010, it was estimated that one team per 140,000 inhabitants was needed; this would mean around 57 teams in Austria (ÖBIG, 2004).
The concept of MPTs can easily be and has been implemented in other countries as well. However and as always, this is depending on political will, financial resources, and organisation of the existing health and social sector.
Worin bestehen die Stärken und Schwächen der Initiative?
Strengths
- Due to the multi-professional composition, flexibility, and cooperation with other professional sectors, carers and users of MPTs have the potential to bridge crucial gaps in LTC systems.
- Patients and their personal preferences are intensely integrated and respected when setting up an individual care and support plan.
- A political commitment for the national implementation and future expansion of services by MPTs exists in Austria.
- Additionally, hospice and palliative services have a quite strong representation in their national umbrella organisation Hospiz Österreich.
Weaknesses
- Current MPT services are mainly limited to the group of terminally ill people, although they represent a promising role model of care for frail older people in general.
- In some regions/organisations limited possibilities and resources (staffing, financial resources) exist in relation to the demand of services.
Opportunities
- Cooperation with the professional and institutional sector of care provision could still be improved.
- MPTs provide a role model for mobile and multi-professional care teams for frail older people in general.
Threats
- (Possible plans for) Cost accounting on the basis of “kind of intervention” instead of “time spent with the client” would significantly reduce the quality and basic idea of individual services.
- Lack of money (private donations, public funds).
Impressum
Autor: Georg RuppeReviewer 1: Laura Holdsworth
Reviewer 2: Anja Dietrich
Verified by:
Externe Links und Literatur
- Joanneum Research (2008), Mobiles Palliativteam Graz. Berechnung der finanziellen Verschiebungspotenziale. Graz: Joanneum Research ForschungsgesellschaftmbH.
- Kratschmar A. & H. Teuschl (2008), Hospiz- und Palliativführer Österreich. Wien: Bundespressedienst.
- Pelttari L., Zottele L. & A. Pissarek (2011), Datenerhebung 2010 Hospiz Österreich. Wien: Dachverband Hospiz Österreich.
- ÖBIG (2004), Abgestufte Hospiz und Palliativversorgung in Österreich. Wien: ÖBIG.
- ÖBIG (2007), Abgestufte Hospiz und Palliativversorgung. Wien: ÖBIG.
- Hospiz Österreich

